Testicular cancer or germ cell tumors are treated with different surgical options like Orchidectomy, RPLND and Testis-Sparing Surgery at Aashray.
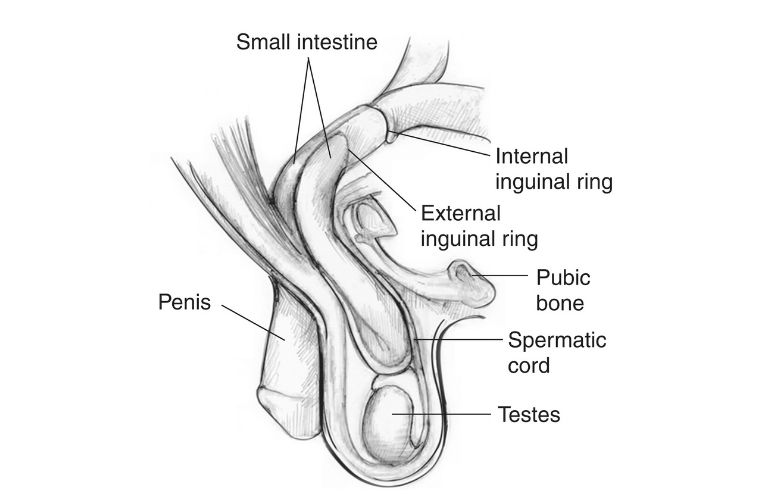
The male reproductive system includes 2 testicles and they are located under the penis in the scrotum. The main function of testicles or testes is to produce sperms and testosterone hormone.
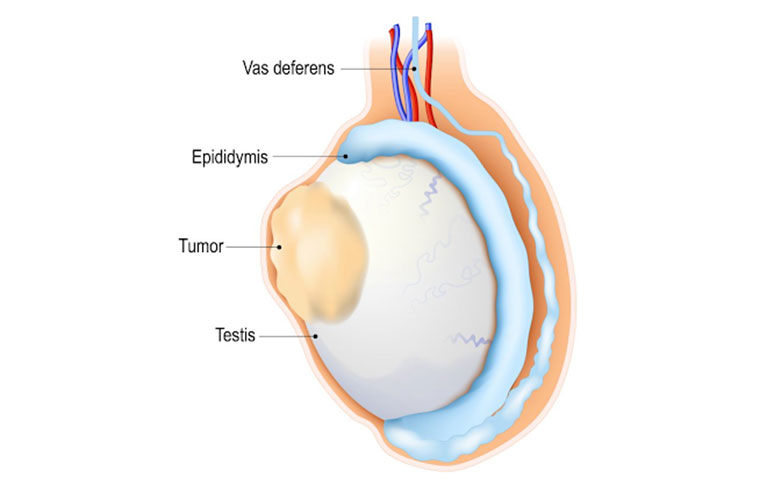
Testicular cancer primarily develops from the germ cells (cells that produce sperms) and these are known as germ cell tumors. There are some uncommon types of testicular cancer which are mentioned later on.
The following are the risk factors for testicular cancer -
People of any age can develop this cancer; however, it is most commonly found in people between the age of 20 to 45.
It is a condition in which one or both the testicles haven’t descended before birth and this condition significantly increases the risk of developing testicular cancer. If this condition is treated in childhood early on, one may lower the risk of developing testicular cancer.
Anyone with a family history of testicular cancer has an increased risk of developing testicular cancer.
Testicular cancers may be of Germ cell or non-germ cell variety.
The 2 main types of germ cell tumors in the testicles are -
A germ cell tumor is called seminoma when it does not include the following types of tumor: Choriocarcinoma, Embryonal carcinoma, Yolk sac tumor, and Teratoma. And a tumor is called a seminoma when it is 100% seminoma. Seminoma has slow growth and does not spread easily.
A germ cell tumor is called non-seminoma when it contains at least one of the following types of the tumor either separately or in combination and the types of tumor are Choriocarcinoma, Embryonal carcinoma, Yolk sac tumor, and Teratoma. Non-seminoma comparatively grows faster and spreads quicker.
The following are the uncommon types of testicular cancer - Leydig cell tumor, Sertoli cell tumor, Carcinoma of the rete testis, and Testicular lymphoma.
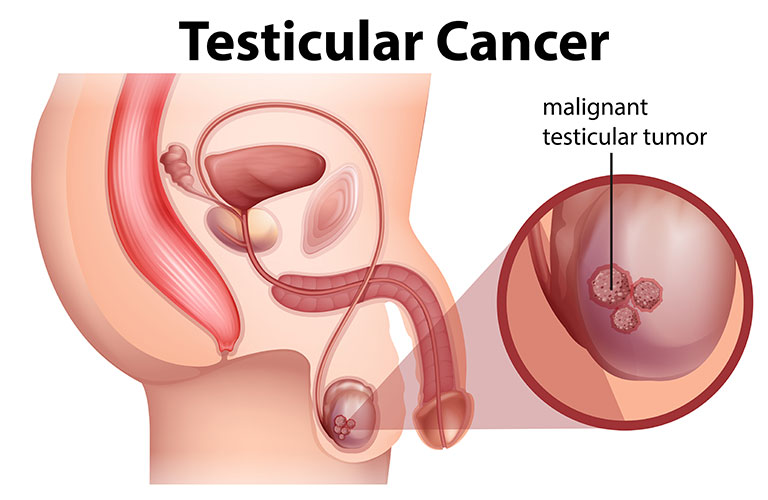
People with testicular cancer may or may not have all the symptoms and in some cases, one may have similar symptoms but for a different medical condition. So, it is to be noted that the symptoms are not a confirmation of cancer. The symptoms of testicular cancer are as follows:
In late stages of testicular cancer, symptoms like:
Staging basically means determining the cell type, location of cancer, and checking if it has spread. Staging helps to determine the best suitable course of treatment for the patient. The stages for testicular cancer are as follow:
This is also called “Germ Cell Neoplasia In Situ (GCNIS)”. This is not really cancer, but a warning that cancer could grow. GCNIS may be found in the seminal tubules and nowhere else.
Cancer is found only in the testicle. It has not spread to nearby lymph nodes.
Cancer has spread to one or more lymph nodes in the abdomen (belly). It has not spread to other parts of the body.
Cancer has spread beyond the lymph nodes in the abdomen. Cancer may be found far from the testicles, like in distant lymph nodes or the lungs. Tumor marker levels are high.
As in the early stages, there are many physical symptoms of testicular cancer, it is always recommended to do a self-exam. It is recommended to do it while standing after a bath. The self-exam includes checking the firmness, texture, and size of testicles, feeling the different contents of scrotum and noticing any changes in it, finding lumps, swelling, or any other abnormalities like pain etc.
Ultrasonography of the scrotum and in some cases, MRI or other scans will be done to evaluate the contents of scrotum and other parts of the body like chest, abdomen etc. to check if cancer has spread to them.
There are many treatment options available for testicular cancer and the treatment is decided based on the results of the diagnosis and several medical tests as well as the overall health and requirements of the patient.
This is basically a way to actively look for changes or abnormalities with normal check-up methods like a physical exam, tumor marker tests, and imaging tests. Surveillance maybe recommended for some Stage 0 cancers.
Surgical options are mainstream for testicular cancer and there are multiple surgeries available for it. However, before one considers getting surgery, changes in semenalysis resulting in diminished fertility and other such issues should be discussed with the doctor.
The further course of treatment will entirely depend upon the biopsy report of removed testis and the results of imaging studies and tumor markers. Active surveillance is mandatory after the surgery to detect the signs of recurrence.
Active surveillance is a must after TSS to detect cancer in case it returns. Side effects like infertility may also be experienced after TSS.
As RPLND has a high chance of recurrence and also depending on the type and location of cancer, surveillance and chemotherapy are recommended after the surgery.
This treatment is used for seminoma-cell cancers to kill cancer cells on the testis or in nearby lymph nodes. It is not recommended for non-seminomas as they are generally resistant to radiation. Few types of radiation are used in this treatment and it is a good option to treat cancer that has spread to other organs/ parts of the body.
In this treatment, medications are used either separately or in the combination with another drug to kill the cancer cells. These drugs travel in the bloodstream and by causing side effects, they kill the cancer cells that may have traveled to lymph nodes. Chemotherapy is recommended for cancers that have spread to the other parts of the body, if tumor markers rise after surgery, and to lower the risk of cancer coming back after surgery.
The follow-ups are especially important in cases of cancers to manage side-effects and monitor the overall health, recovery progress as well as check for any signs that cancer has come back. So, follow-up care and active monitoring are essential. These include regular physical examinations, imaging tests and blood & tests. Along with professional help, it is important to learn and do testicular self-exam often. People who had testicular cancer usually receive follow-up screening for at least 10 years after their treatment ends.
Cancer rehabilitation and survivorship care are recommended, and this could mean any of a wide range of services that help people regain control over many aspects of their lives and remain as independent and productive as possible and these services may include physical therapy, career counseling, pain management, nutritional planning, financial counseling, and/or emotional counseling.


Dr. Ashit Shah is a senior consultant Urologist heading Aashray Urology Institute. After completing his M.B.B.S. and M.S. in General Surgery, he was awarded Diplomate of National Board (D.N.B.) in Genito-Urinary Surgery by the National Board of Examinations, New Delhi. He earned his Diplomate in Laparoscopic Urology from Louis Pasteur University, Strasbourg, France in the year 2006. Dr. Shah has a special interest in Endo-Urology, especially Urolithiasis i.e. Urinary Stone Disease. Having spent more than 27 years in the profession of Urology, he has experience of over 75,000 urological consultations and more than 15,000 surgeries. Being counted amongst the torch bearers of ethical and transparent medical practice in the city of Vadodara, he was conferred ‘Inspiring Urologist Award’ for the year 2019 by The Economic Times.